
Over the past decade, there has been an increase in discussions involving industry stakeholders, regulatory agencies, and physicians about developments in the emerging microbiome therapeutics industry. The field initially triggered inquiries and these conversations have since evolved, indicating a noticeable positive shift in attitudes over time.
The recent FDA approvals of two microbiome products in the US, in
Considering these developments, there is now strong recognition of the potential benefits offered by microbiome treatments.
Deviation from traditional approaches
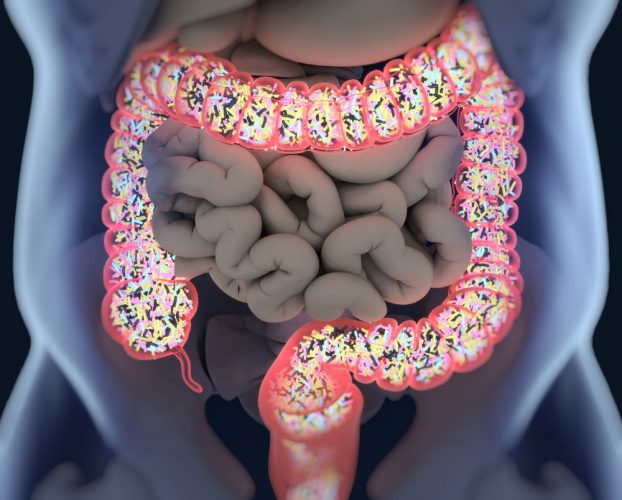
Microbiome therapeutic development differs from traditional chemical agents, involving the use of live organisms and complex communities of micro-organisms. This unique mode of action offers potential with proven efficacy, however, given its complexity, also requires an updated approach for overall risk management.
Engaging in continuous dialogue with regulatory bodies in
During the development of clinical trials that use faecal-derived material, the necessity of safety is paramount. Implementing stringent specifications, not only guarantees the safety of the product but also ensures reproducible quality and efficacy.
For example, before stool is collected, donors are screened, taking various samples of blood and faecal matter to check for several harmful bacteria, including multi-resistant bacterium or pathogenic bacterium. These methods also acknowledge the necessity of adapting to external environmental changes, as evidenced by successful adjustment in screening for COVID-19 after the pandemic started.
When collecting stool, experts will also consider the amount of microorganisms present, and their potential variety and diversity, to understand the overall health and function of the individual donor's microbiome.
Pooling as a promising "next generation" solution
Each gut microbiome is intricate and unique, shaped by the diverse compositions of microorganisms and the inherent individuality within each microbiome. Notably, from one donor to another, significant variations exist. While this approach has shown to be safe and efficient in Clostridium difficile, the variability between donors may lead to random outcomes and responses in patients for immune-mediated diseases. Therefore, understanding and addressing the complexities of individual gut microbiomes are crucial for ensuring the safety and reliability of microbiome-based therapeutics.
Thus,
Advancing microbiome innovation
The future of microbiome therapy will be marked by the developments of new treatments across a multitude of disease areas beyond C. difficile infection, especially in oncology”
The future of microbiome therapeutics will be marked by the developments of new treatments across a multitude of disease areas beyond C. difficile infection, especially in oncology. For example, numerous publications have highlighted the role of the gut microbiome in improving the efficacy and diminishing the toxicity of chemotherapeutic drugs.4
Notably, microbiome therapies have strong potential in onco-haematology, where antibiotic and chemotherapy-derived loss of gut diversity is predictive of mortality in patients who have undergone an allogeneic haematopoietic stem cell transplant, as well as GvHD occurrence and infection.5 Therefore, using microbiome therapies in this context could be promising in limiting infection and improving patients' overall survival. This is the approach that we have chosen for our second drug candidate MaaT033, currently being evaluated in a Phase II trial in
Microbiome therapeutics: microscope to medicine:
Catch up on the previous articles in this series here.
Potential of microbiome therapeutics in graft-versus-host disease
In GvHD, and for patients who have failed earlier treatment lines, microbiome therapies can introduce a novel therapeutic approach by restoring the gut microbiome ecosystem and helping maintain the patient’s immune function, without compromising it excessively, therefore reducing the risk of infectious complications and relapse. This could offer a distinct immuno-restorative option that could complement standard immunosuppressive drugs and could become a potential breakthrough for patients with no therapeutic options.
microbiome therapies…could offer a distinct immuno-restorative option that could complement standard immunosuppressive drugs and could become a potential breakthrough for patients with no therapeutic options”
Additionally, recent studies have started to shed a wider light on the role of the gut microbiome, linking abnormalities to diseases such as amyotrophic lateral sclerosis (ALS). The link between gut microbiota and ALS first emerged from preclinical evidence, then from clinical observations indicating a disease-modifying role for the gut microbiome.
Accelerating access to microbiome therapeutics
Early Access Programs (EAPs), play a crucial role in advancing the microbiome therapeutics landscape and contributing to its potential future, offering a pathway to address unmet medical need, provide potential solutions for patients who may not qualify for traditional clinical trials, and for those who cannot afford to wait the lengthy process of traditional drug development. The significance of EAPs also lie in their ability to harness real-world data, offering insights into the effectiveness and safety of emerging therapies.
While clinical trials can provide evidence for the safety and efficacy of a medical product in a controlled environment, vital data for how a new medicine will perform in the real world is often lacking. EAPs should therefore be considered both important and complementary to clinical trials, allowing pharmaceutical companies to gain a better understanding of how patients respond to treatments outside of a controlled, clinical environment. This can involve a broader range of patients, including those with diverse health profiles and medical histories, enabling a more comprehensive understanding of treatment responses and potential variations in efficacy and safety.
Shifting our focus from immune suppression to immune restoration is a novel mode of action, which offers the potential to reduce infections and complications compared to traditional approaches”
For instance, results from a recent European EAP using MaaT013, a pooled-donor microbiome ecosystem therapy, indicate its safety and demonstrate a high gastrointestinal overall response rate (GI-ORR) in refractory acute GvHD patients (54 percent at day 28).
Positive responses significantly impact overall survival, especially in individuals unresponsive to current treatments (67 percent for responders vs. 24 percent for non-responders). Using MaaT013 as a third line of treatment, post corticosteroid and ruxolitinib failure, resulted in a GI-ORR of 61 percent at 28 days (81 percent for responders vs. eight percent for non-responders).
Microbiome therapeutics: a new era
The microbiome sector offers a new and exciting way of looking at how we can treat disease. Shifting our focus from immune suppression to immune restoration is a novel mode of action, which offers the potential to reduce infections and complications compared to traditional approaches and provides groundbreaking treatment options across a realm of serious and often neglected diseases, from metabolic to neurologic and inflammatory diseases.
There will be challenges to overcome with any emerging field of research, but the potential for transformative progress inspires hope, and allows us to remain curious and optimistic for what lies ahead in the future of microbiome therapeutics.
About the author
References
US FDA approves Ferring's Rebyota for Clostridioides difficile infection. [Internet] Pharmaceutical Technology. 2022. [cited 2024Feb]. Available from: https://www.pharmaceutical-technology.com/news/fda-ferring-rebyota-cdi/- FDA Approves First Orally Administered Fecal Microbiota Product for the Prevention of Recurrence of Clostridioides difficile Infection 2024. [cited 2024Feb]. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-first-orally-administered-fecal-microbiota-product-prevention-recurrence-clostridioides
- Malard F, Loschi M, Huynh A, et al. Pooled Allogeneic Faecal Microbiota MAAT013 For Steroid-Resistant Gastrointestinal Acute Graft-Versus-Host Disease: A Single-Arm, Multicentre Phase II trial. eClinicalMedicine. 2023; 62:102111.
- Oh B, Boyle F, Pavlakis N, et al. Emerging Evidence Of The Gut Microbiome In Chemotherapy: A Clinical Review. Front. Oncol. 2021;11.
-
Peled JU, Hanash AM, Jenq RR. Role of The Intestinal Mucosa In Acute Gastrointestinal GVHD. Blood. 2016;128(20):2395-402; Staffas A,
Burgos da Silva M , van den Brink MR. The Intestinal Microbiota In Allogeneic Hematopoietic Cell Transplant And Graft-Versus-Host Disease. Blood. 2017;129(8):927-33; Taur Y, et al. The Effects Of Intestinal Tract Bacterial Diversity On Mortality Following Allogeneic Hematopoietic Stem Cell Transplantation. Blood. 2014;124(7):1174-82; Jenq RR, Taur Y, Devlin SM, et al. M. Intestinal Blautia Is Associated With Reduced Death From Graft-Versus-Host Disease. Biol. Blood and Marrow Transplantation. 2015;21(8):1373-83.
The post Advancing microbiome innovation appeared first on European Pharmaceutical Review.
© Russell Publishing Limited, 2024. All Rights Reserved., source


