Magellan Rx Management, a division ofMagellan Health, Inc. (NASDAQ: MGLN), today announced annualized savings of over $40 million for five health plan customers who were early adopters of its oncology biosimilar medical benefit drug management solution. This comprehensive approach encourages the use of oncology therapeutic biosimilars over more expensive reference products, when clinically appropriate. Savings figures are expected to grow even further as more customers have adopted the program since its inception and the market shift to biosimilars accelerates.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20210609005124/en/
Magellan Rx Management (Grapic: Business Wire)
“Magellan Rx continues to be a market leader and disrupter in delivering leading-edge solutions for the evolving healthcare landscape, and our health plan partners are recognizing real savings through these programs while maintaining a high quality level of care for their members,” said Steve Cutts, PharmD, senior vice president and general manager, specialty, Magellan Rx Management. “We have been tracking the emergence of biosimilars and started to deliver biosimilar-first solutions as early as 2016. It’s our commitment to staying ahead of the trend that has made us a trusted partner in medical benefit management for nearly two decades.”
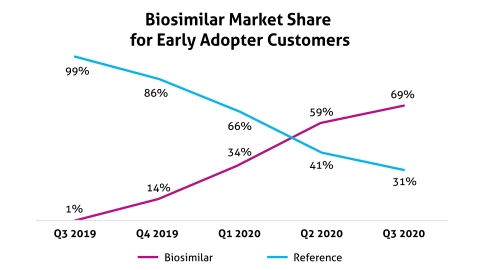
Health plan customers implemented the program, which focuses on promotion of biosimilars for three oncology products, on or before January 1, 2020. Most of the current savings were achieved with the first two products that had biosimilar availability (see graphic), and preliminary results with the third product are promising. According to Magellan Rx’s internal data, these biosimilars can cost payers up to 40% less than their respective reference brands.
“We knew we wanted to collaborate with a medical pharmacy expert,” said Carly Rodriguez, pharmacy director at Moda Health, a health plan that implemented the program with success. “We were looking for a partner that would do more than save our plan on rising specialty costs, but that would continue to support our members with Moda’s signature quality of care. In partnering with Magellan Rx, we know we have the right experts on our side and we anticipate expanding the program to additional biosimilar agents, as clinically appropriate.”
These positive results, after just one year, reflect the growing need for management programs that deliver lower cancer treatment costs for payers and patients while maintaining high standards of care. Magellan Rx develops cost-effective and leading-edge strategies for medical benefit drug management across several categories, offering flexible solutions that can also operate outside of the traditional payer-PBM relationship. Health plans can leverage the extensive clinical expertise and experience at Magellan Rx by delegating specialty and medical drug management services while retaining a separate PBM. Read more about Magellan Rx’s total specialty drug management solutions. To learn more about Magellan Rx Management’s history of biosimilar management, visit, Magellan Insights.
About Magellan Rx Management: Magellan Rx Management, a division of Magellan Health, Inc., is a next-generation pharmacy organization that is delivering meaningful solutions to the people we serve. As pioneers in specialty drug management, industry leaders in Medicaid pharmacy programs and disruptors in pharmacy benefit management, we partner with our customers and members to deliver a best-in-class healthcare experience.
About Magellan Health: Magellan Health, Inc. is a leader in managing the fastest growing, most complex areas of health, including special populations, complete pharmacy benefits and other specialty areas of healthcare. Magellan supports innovative ways of accessing better health through technology, while remaining focused on the critical personal relationships that are necessary to achieve a healthy, vibrant life. Magellan's customers include health plans and other managed care organizations, employers, labor unions, various military and governmental agencies and third-party administrators. For more information, visit MagellanHealth.com.
(MGLN-GEN)
View source version on businesswire.com: https://www.businesswire.com/news/home/20210609005124/en/

