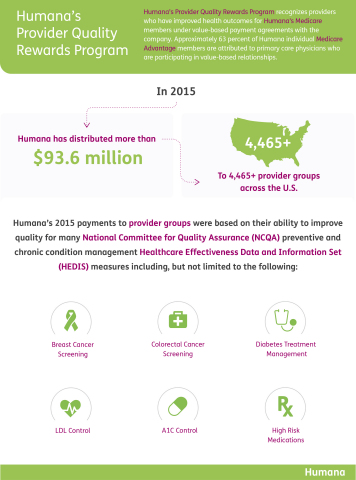
Humana Inc. (NYSE: HUM) today announced that it distributed more than $93.6 million to approximately 4,465-plus provider groups across the United States who participate in Humana’s Provider Quality Rewards Program.
This Smart News Release features multimedia. View the full release here: http://www.businesswire.com/news/home/20161116006150/en/
Humana Distributes More Than $93 Million in Quality Payments to Providers Nationwide (Graphic: Business Wire)
“This year’s payments suggest that physicians who provide care in value-based relationships continue to experience success,” said Chip Howard, Humana’s Vice President of Payment Innovation in the Provider Development Center of Excellence. “Physicians participating in our value-based programs are making significant strides in improving their patients’ health and care experience.”
Humana has paid physicians for quality care outcomes since 2012, reflecting the company’s continued efforts to support physicians in their transition from fee-for-service to value-based reimbursement models. Approximately 63 percent of Humana individual Medicare Advantage members are affiliated with primary care physicians who are participating in value-based relationships.
Humana’s Provider Quality Rewards Program is part of the company’s value-based initiative, which is focused on promoting evidence-based, high-quality care. The initiative recognizes physician group preparedness for value-based arrangements by offering several levels of participation through programs including Star Rewards, Model Practice, Medical Home and shared savings/full value programs for value-based care.
“As the industry continues to shift toward value-based payment, programs such as these are proving that care tied to quality metrics can have a meaningful impact on a patient’s health,” said Dr. Roy Beveridge, Humana’s Chief Medical Officer. “Physicians are benefitting, too, by being paid for the complex care they are delivering.”
Approximately 4,465 physician groups received payments from Humana in recognition of improved outcomes for Humana’s Medicare members made during 2015. Reward settlement finalization takes place in 2016 for the 2015 Provider Quality Rewards Program to allow time for final claims and supplemental data submission.
Humana’s 2015 payments to providers were based on their ability to improve quality for many National Committee for Quality Assurance (NCQA) preventive and chronic condition management Healthcare Effectiveness Data and Information Set (HEDIS) measures including, but not limited to the following:
- Breast cancer screening
- Colorectal cancer screening
- Diabetes treatment management
- LDL control
- A1C control
- High-risk medications
Earlier in November, Humana announced care quality outcomes for approximately 1.2 million Medicare Advantage members affiliated with providers in value-based reimbursement model agreements with Humana. The results showed improvements across categories such as medical costs, chronic condition management, and improved HEDIS scores.
Approximately 1.8 million of Humana’s individual Medicare Advantage members are cared for by approximately 49,600 primary care physicians in more than 900 value-based payment relationships across 43 states and Puerto Rico. For more information, visit humana.com/valuebasedcare.
About Humana
Humana Inc., headquartered in Louisville, Ky., is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care. The company’s strategy integrates care delivery, the member experience, and clinical and consumer insights to encourage engagement, behavior change, proactive clinical outreach and wellness for the millions of people we serve across the country.
More information regarding Humana is available to investors via the Investor Relations page of the company’s web site at www.humana.com, including copies of:
- Annual reports to stockholders
- Securities and Exchange Commission filings
- Most recent investor conference presentations
- Quarterly earnings news releases
- Calendar of events
- Corporate Governance information
View source version on businesswire.com: http://www.businesswire.com/news/home/20161116006150/en/


